Background: In 2022, two new acute myeloid leukemia (AML) classifications (World Health Organization, WHO and International Consensus Classification, ICC) and a new edition of the European LeukemiaNet (ELN) prognostic system have been released. These advances have been driven by the need to incorporate molecular characterization into the diagnosis and management of AML.
Although important similarities in the diagnostic classifications have been recently recognized by diverse validation studies, the different approach to define AML ontogenesis (primary vs secondary) remains a central issue of the classification discrepancy. While for the WHO 2022 a prior diagnosis of myelodysplastic syndrome (MDS) or MDS/myeloproliferative neoplasm (MPN) is sufficient to define AML myelodysplasia-related (MR), the ICC no longer recognizes the AML arising from MDS (sAML) as a disease entity, and instead introduces a list of “diagnostic qualifiers”, also including therapy-related AML (tAML). Nevertheless, whether these “diagnostic qualifiers” represent a mere “descriptive” information or impact on prognosis and outcome is not well defined.
Methods: We studied a cohort of 936 AML patients collected through a multicenter international collaboration across 5 academic centers. An integration of clinical and cytogenetic/molecular data was used to apply the WHO 2016, WHO 2022 and ICC diagnostic classifications and the 2017 and 2022 edition of ELN prognostic risk stratification criteria.
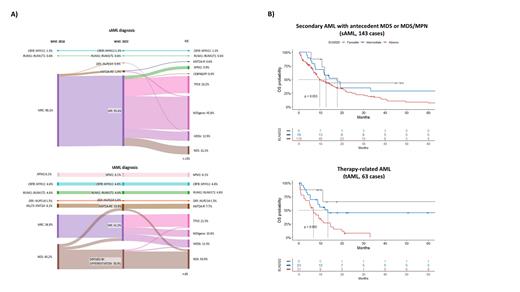
Results: Overall,220 cases were classified as secondary AML (155 sAML and 65 tAML). As per the2016 and 2022 WHO editions, the majority of sAML cases, accounting for 98.1% and 95.5% respectively, fell into the myelodysplasia-related changes (MRC) AML and AML-MR categories due to the “disease defining” presence of an antecedent MDS or MDS/MPN. According to the ICC, 81.9% of sAML cases were defined by the presence of a MDS-related genetic profile, belonging to AML with mutated TP53 (AML- TP53) and AML with MDS-related gene mutations (AML-MDSgene) and cytogenetic abnormalities (AML-MDSk) subcategories.
The tAML group showed a greater diagnostic heterogeneity, with a higher frequency of KMT2A-related categories (10.8% and 7.7% according to WHO 2022 and ICC, respectively) and AML- TP53 for the ICC (21.5%, Fig. 1A).
In terms of outcomes, according to the ELN 2022 risk classification the sAML and tAML groups were classified into favorable risk 5.8% and 13.9%, intermediate 12.3% and 36.9%, and adverse 81.9% and 49.2%, respectively. Notably, while the ELN 2022 edition was effective in stratifying the group of tAML patients receiving conventional treatment (p=0.002), no statistically significant differences were noticed when sAML patients were stratified based on the same ELN 2022 risk categories ( Fig. 1B).
We then compared our sAML cohort to AML cases with ICC MDS-related profile not fulfilling the anamnestic criterion of a prior MDS diagnosis (233 cases, 32.54% - AML- TP53/MDSgene/MDSk subcategories), in terms of molecular characteristics and outcome. Remarkably, both groups showed a similar prevalence of MDS genes, except for RUNX1, which was more frequent in the AML cases with the ICC MDS-related profile (14%) than in sAML (6.3%, p =0.034). Finally, both groups showed similar outcomes.
Conclusions: Here, we demonstrated the overarching importance of the biological ontogenetic profile in AML (>80% of sAML presented an MDS-related profile) and of the risk stratification according to the new classifications (>80% of sAML belonged to adverse ELN 2022 risk). As to outcomes, 2022 ELN edition confirmed its stratification capability for tAML, while sAML were not adequately stratified. This evidence supports the idea that therapy-related AML should be acknowledged and classified as “second” neoplasms, rather than being categorized as secondary AML. Considering the overlap in AML of MDS-related profile regardless of the presence of an antecedent diagnosis of MDS as “diagnostic qualifier”, these cases could potentially benefit from treatments specifically tailored for MDS-related conditions or those typically reserved for secondary AML, such as CPX-351.
Disclosures
Venditti:Medac: Consultancy; Janssen: Consultancy, Honoraria, Other: travel support ; AbbVie: Consultancy, Honoraria, Other: travel support ; Jazz: Consultancy, Honoraria, Other: travel support ; Amgen: Consultancy, Honoraria, Other: travel support ; Pfizer: Consultancy, Honoraria, Other: travel support , Speakers Bureau; Novartis: Consultancy, Honoraria, Other: travel support . Maciejewski:Regeneron: Consultancy, Honoraria; Alexion: Membership on an entity's Board of Directors or advisory committees; Novartis: Honoraria, Speakers Bureau; Omeros: Consultancy. Voso:Celgene/BMS: Other: Advisory Board; Jazz: Other: Advisory Board; Abbvie: Speakers Bureau; Jazz: Speakers Bureau; Celgene/BMS: Research Funding, Speakers Bureau; Novartis: Research Funding; Astra Zeneca: Speakers Bureau; Novartis: Speakers Bureau; Astellas: Speakers Bureau; Syros: Other: Advisory Board.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal